Why your claims with x-rays are being denied and what you can do
Some procedure codes require the submission of documentation with claims for Delta Dental PPO™ and Delta Dental Premier® patients. Let’s review radiographic image requirements for common procedures and the associated denials that can occur.
Crowns
Pre-operative and periapical (depicting the apex) radiographic images are required when submitting crown procedures D2710 through D2794. Do not substitute a panoramic radiograph to replace periapical images. Radiographs must show the endodontic and periodontal state of the tooth and must be taken within one year of the crown prep procedure.
Photographs must accompany radiographs when evidence of necessity is not obvious on the radiographs.
Lab slips should be maintained as part of the patient record.
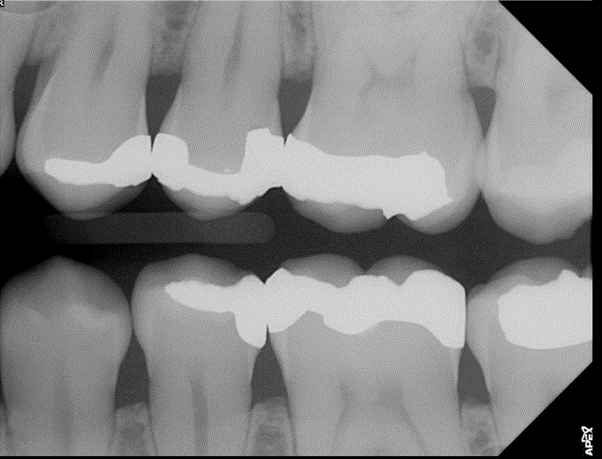
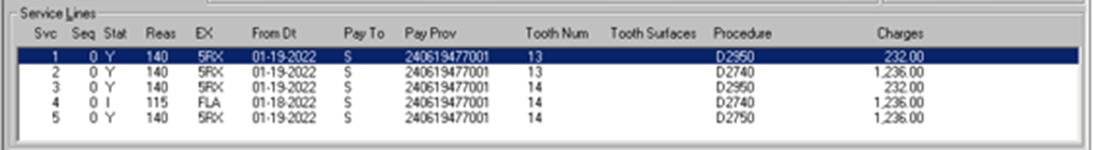
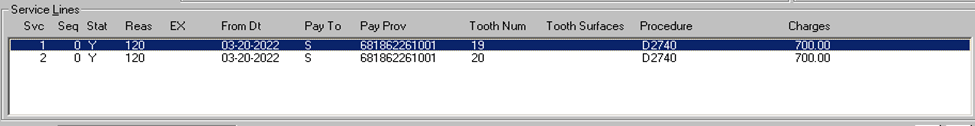
In this example, the following radiographic images fail to depict the entire tooth. Pre-operative radiographic images must show the apex (tip of the tooth’s root) and are requested to rule out associated periapical pathology.

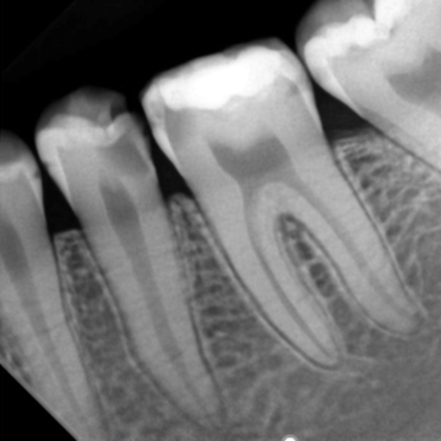
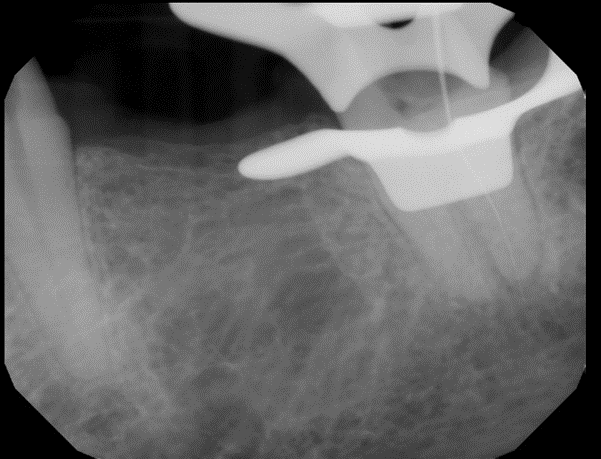
In comparison, the following radiographic image correctly depicts the apices of the submitted teeth.
Common reasons for crown denials
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5RX. Benefits could not be determined because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
Core buildup, including any pins
Periapical radiographs taken within one year of the planned treatment are required when submitting core buildup and post and core procedures D2950 through D2957.
Do not substitute a panoramic radiograph to replace periapical images.
A narrative is also required. Per the American Dental Association, build-ups should not be reported when the procedure only involves a filler to eliminate any undercut, box form, or concave irregularity in the preparation.
Common reasons for core buildup denials
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5RX. Benefits could not be determined, because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
- 564. Submit clinical treatment narrative.
- 5BU. The fee for buildups is included in the fee for the completed restoration unless there is extensive loss of tooth structure.
Endodontics
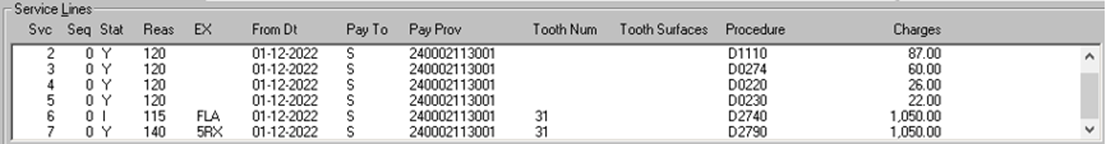
Pre-operative and post-operative periapical radiographs are required when submitting endodontic procedures D3310 through D3330 and D3921. All radiographs, including working radiographs, should be maintained in the patient treatment record.
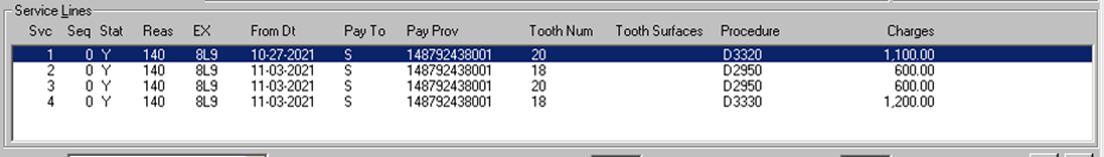
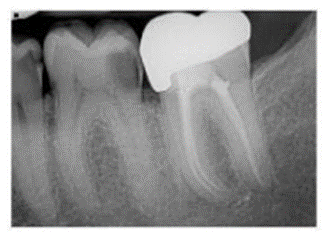
The following radiographic image fails to depict completed root canal therapy on the submitted teeth.
In contrast, the following radiographic images correctly depict an acceptable pre-operative periapical x-ray and post-operative x-ray of completed root canal therapy on the submitted tooth.

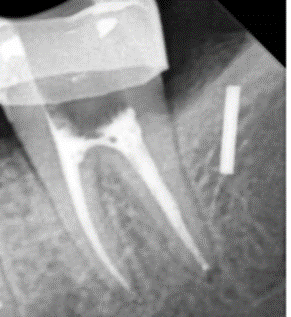
In this second example, the following radiographic images correctly depict an acceptable pre-operative periapical x-ray and post-operative x-ray of completed root canal therapy on tooth #19.

If your endodontic claim is denied, you may see one of the following denial codes:
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- FMW. Benefits could not be determined because of missing pre- and post-operative periapical images.
- 8L9. Benefits could not be determined because of missing post-operative radiographic images of completed root canal therapy.
- 5RX. Benefits could not be determined, because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
Periodontics, including scaling and root planning
When submitting periodontic procedures D4210 through D4212, D4240 through D4245, D4260 through D4285, D4341 through D4342 or D4381, you must include bitewing radiographs taken within 12 months of the planned treatment that show both arches of bone levels. Furthermore, loss of alveolar crest height beyond the normal 1-1.5-millimeter distance to the cementoenamel junction (CEJ) must be evident on radiographs. Periapical or panoramic radiographs can only be substituted when bone loss exceeds levels that can be captured in a vertical bitewing.
Other requirements include periodontal charting (probing) completed within the past 12 months, periodontal case type and diagnosis with detailed clinical chart notes regarding the necessity of the periodontal treatment.
The following bitewing x-ray is nondiagnostic, as the interproximal contacts are overlapped and fail to show bone loss.
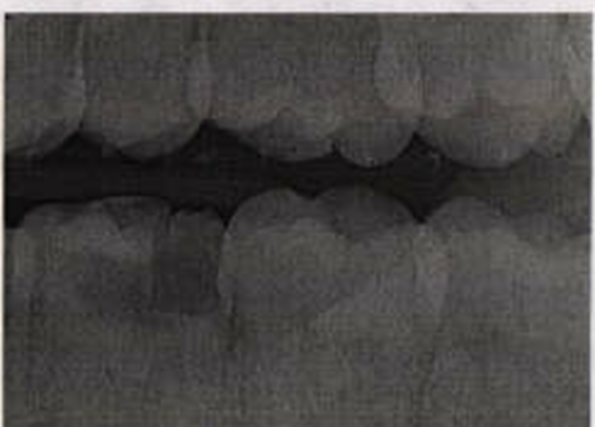
Compare this to the following bitewing x-ray, which depicts both appreciable bone loss and calculus.

Common reasons for periodontic denials
- Benefits could not be determined because of missing full-mouth radiographic images. (Note: This code may also be used to request bitewing x-rays.)
- 5F5. Submit dated pre-operative diagnostic radiographs, current periodontal chart, dated appointment schedule and clinical treatment notes.
- 426. Benefits could not be determined because of missing radiographic images, periodontal charting and treatment record.
- 5GB/5GC. Submit current periodontal chart, dated pre-operative diagnostic radiographs and a copy of the patient treatment record.
- 574. Benefits could not be determined because of missing periodontal charting.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
- 5GJ. Submit dated copy of the original treatment notes.
- 5F8. Submitted documentation fails to support payment of benefits for scaling and root planing.
Crown lengthening
Pre-treatment bitewing radiographs taken within 12 months of the planned treatment are required when submitting for the crown lengthening procedure (D4249).
A detailed clinical narrative is also required.
When procedure D4249 is performed on the same day as the preparation/placement of the crown, a separate fee for procedure D4249 may not be charged to the patient or Delta Dental. Prior to final restoration of a tooth, a minimum of four weeks must be allowed following clinical crown lengthening.
Common reasons for crown lengthening denials
- 573. Benefits could not be determined because of missing full-mouth radiographic images. (Note: This code may also be used to request bitewing x-rays.)
- 564. Submit clinical treatment narrative.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
- 9WA. The fee for this procedure is considered to be part of and included in the fee for a completed service.
Implant supported prosthetics
You are required to include current periapical radiographs, including the apex of the implant body and surrounding bone, when submitting for implant-supported prosthetic procedures D6055 through D6077, D6082 through D6088, D6094, D6097 through D6099, D6110 through D6123 and D6194 through D6195.
Do not substitute a panoramic radiograph to replace periapical images. Pre-operative x-rays depicting each implant site are required to determine payment of benefits on pre-authorizations. We must receive post-operative x-rays of implant placement to determine payment of benefits on paid claims. These x-rays must depict the entire implant.
Photographs, if available, may also be submitted for review.
For example, the following panoramic radiographic x-ray is nondiagnostic. It fails to clearly depict implant placement at site #9. Do not substitute a panoramic radiograph to replace periapical images.
The following post-operative periapical x-ray, however, correctly depicts the apex of the implant body and surrounding bone.

Common reasons for implant-supported prosthetic denials
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 586. Benefits could not be determined because of missing post-operative radiographic images.
- 5RX. Benefits could not be determined, because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
Fixed prosthodontics (bridge abutment crowns)
When submitting for fixed prosthodontic procedures D6710 through D6794, you are required to include pre-operative periapical radiographs that show the current endodontic and periodontal state of the tooth. These x-rays must be taken within one year of the crown prep procedures. Do not substitute a panoramic radiograph to replace periapical images.
Photographs, if available, may also be submitted.
Lab slips should be maintained as part of the patient record.
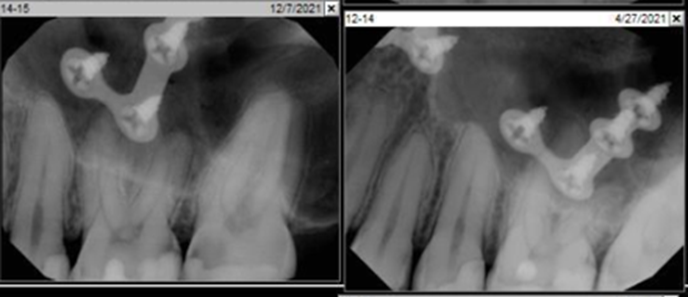
In this example, the radiographic image is nondiagnostic, as it fails to clearly depict the submitted abutment teeth.
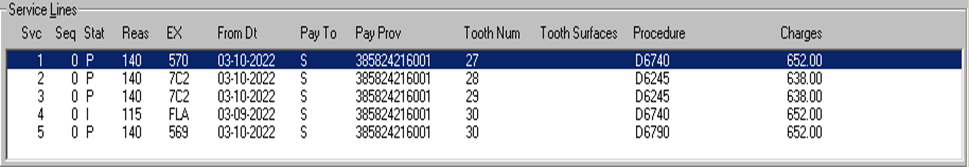
In comparison, the following radiographic images for proposed bridge 13-15 clearly depict abutment teeth #13 and #15.
Common reasons for fixed prosthodontic denials
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5RX. Benefits could not be determined, because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
Oral surgery (impacted tooth)
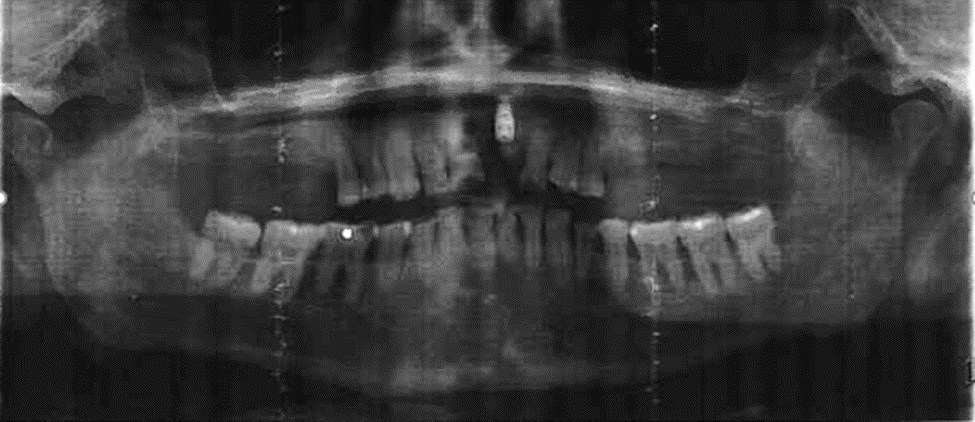
Current periapical or panoramic radiographs are required when submitting oral surgery procedures D7210 through D7241 and D7251. Radiographs are necessary to evaluate conditions detected by history and clinical examination and are essential to detect, diagnose, and treat conditions that otherwise may be difficult to identify.
Further, as the classification of impactions is based on the anatomical position of the tooth rather than the surgical technique employed in removal, preoperative radiographs should be maintained in the patient treatment record.
Detailed, tooth specific clinical chart notes regarding the necessity of the treatment and photographs, if available, should be submitted.
The following panoramic x-ray clearly depicts the anatomical position of the third molars.

Common reasons for oral surgery denials
- 570. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5L8. Benefits could not be determined because of missing pre-operative periapical radiographic images.
- 5T2. Benefits could not be determined because of missing pre-operative panoramic radiographic image.
- 5RX. Benefits could not be determined, because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
General tips for submitting x-rays
To expedite the processing of your claim and to ensure timely benefit determination, always submit the appropriate mounted and dated x-rays and supporting documentation on your initial submission. Enter the required documentation information in the “Remarks” or “Comments” field of the claim.
You can refer tothe Submission Requirements table, which is located on pages 4-1 through 4-3 of the 2022 Claims Processing Policies and Procedures Handbook, to identify the necessary documentation and clinical information required for review of specific procedure codes.Please refer to the specific procedure code in the handbook for more details regarding the description of procedures.
Please do not submit original radiographic images if they are the only diagnostic record for your patient. Duplicate radiographs or radiographic image copies of diagnostic quality, including paper copies of digitized images, are acceptable. We do not return radiographic images or other documentation submitted with paper claims; however, we will make an exception when we receive a stamped, self-addressed envelope with the claim.
During clinical review of claims and pre-treatment estimates, Delta Dental reserves the right to request radiographic images and documentation for procedures that otherwise may be identified as not requiring the submission of documentation.
—
CDT coding and nomenclature are the copyright and a trademark of the American Dental Association, all rights reserved.
Recent posts
- Delta Dental is partnering with dental schools to offer exclusive CE courses
- Drive better patient experiences with benefit conversations
- Offer care beyond the chair with teledentistry
- Healthy mouths begin with hygienists
- How to educate patients and make them partners in oral health
- Dr. Justin Perdichizzi — serving those who served
- Get your patients to make (and keep) their dental appointments
- One sign-on, many advantages
- Delta Dental hosts in-person Provider Advisory Council in Arizona
- Tooth be told, we love our dentists
