Exploring the connection between COVID-19 and oral health
What do oral ulcers and loss of taste have in common? These conditions may be symptoms of COVID-19 that dentists should be aware of.
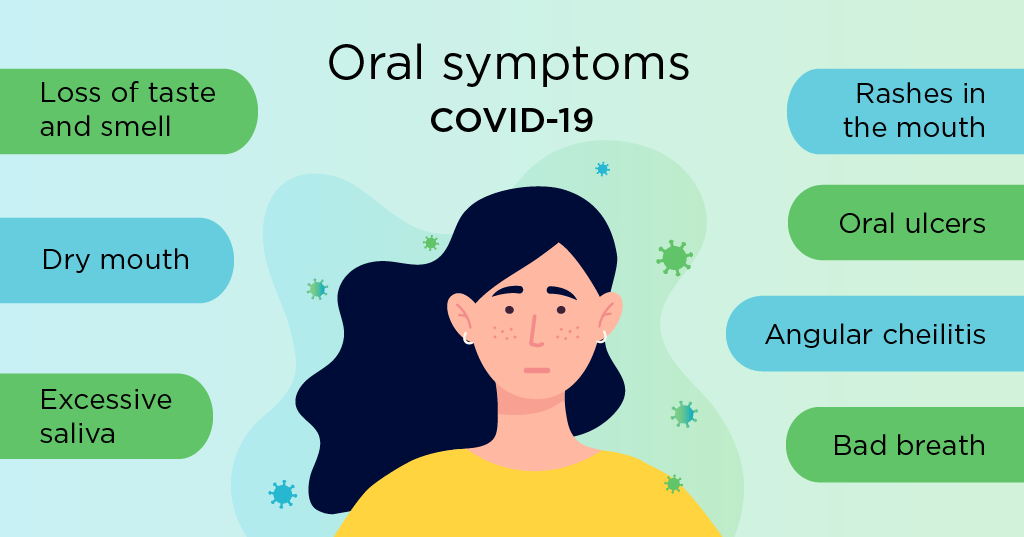
Oral symptoms of COVID-19
- Dry mouth and loss of taste and smell. Dry mouth and loss of taste and smell are two symptoms reported by many COVID-19 patients, according to research published in the American Journal of Otolaryngology (September 2020). These can be some of the first and only symptoms exhibited in some cases.
- Excessive salivation and angular cheilitis. Conversely, hypersalivation is also a potential symptom, according to a case-series and literature review in Oral Diseases (October 2020). Hypersalivation can contribute to issues like angular cheilitis (inflammation of the corners of the mouth), since the salivary enzymes in excess saliva can irritate the skin.
- Bad breath. The SARS-CoV-2 virus can cause changes to the surface of the tongue and the chemicals in saliva. These changes may lead to the development of halitosis (bad breath), according to a letter in Special Care in Dentistry (November 2020). However, more research needs to be done, since there are a variety of factors that can contribute to more noticeable bad breath. For example, wearing a mask may make a patient more aware of the smell of his or her breath or encourage mouth breathing, which can contribute to bad breath. Bad breath is also a common side effect of several over-the-counter medicines used to treat COVID-19 at home.
- Oral ulcers and mouth rashes. Several patients who have tested positive for COVID-19 were also diagnosed with oral ulcers, according to research published in Oral Diseases in May 2020.Another potential symptom is the presence of a rash on the upper palate of the mouth. Various types of internal rash were found in six of 21 patients with confirmed diagnoses of COVID-19, according to a study in JAMA Dermatology (July 2020). Certain rash patterns are more commonly associated with viral infections, and the rashes found in COVID-19 patients are consistent with those patterns.
Gum disease and the severity of COVID-19
Periodontal pockets could be a favorable reservoir for the virus that causes COVID-19, according to research published in Medical Hypotheses (October 2020).
There is also some evidence that inflammation caused by periodontal disease could contribute to the severity of a patient’s COVID-19 symptoms. This is because inflammation prompts the release of interleukin-6 (IL-6), which can damage tissue in the lungs and blood vessels. Damage to these body parts can lessen the amount of oxygen a person gets and contribute to COVID-19 progressing faster.
COVID-19 joins a number of other diseases worsened by the presence of periodontitis, including diseases of the brain, heart and lungs.
Problems with diagnosis
Oral complications because of a COVID-19 infection have been poorly described and potentially underreported, likely due to the fact that most oral symptoms are unlikely to be fatal or dangerous. This has left gaps in the early diagnosis of the onset and characterization of such symptoms, as well as their associations with COVID-19 outcomes.
One of the problems with treating COVID-19 is that two people rarely have the exact same symptoms. Some people infected with the disease may only experience loss of smell, while others experience many other symptoms. Further research will provide a greater understanding of how the coronavirus interacts with the body. As dentists become aware of the variety of oral symptoms associated with COVID-19, they may even be able to use that information to detect otherwise asymptomatic cases in their patients.
Recent posts
- Delta Dental is partnering with dental schools to offer exclusive CE courses
- Drive better patient experiences with benefit conversations
- Offer care beyond the chair with teledentistry
- Healthy mouths begin with hygienists
- How to educate patients and make them partners in oral health
- Dr. Justin Perdichizzi — serving those who served
- Get your patients to make (and keep) their dental appointments
- One sign-on, many advantages
- Delta Dental hosts in-person Provider Advisory Council in Arizona
- Tooth be told, we love our dentists
